The infections that resist the effect of antibiotics are one of the most serious threats to the public health world. A new study, conducted by researchers at the Oxford Universityin the United Kingdom, suggested a new warning for the development of future treatments against bacterial infections.
To deal with the problem of antibiotics that are not effective, the use of drugs known as “antimicrobial peptides”. These are compounds produced naturally by most living organisms, including animals, and play an important role in the innate immunitywhich is the first line of defense against bacterial infections.
However, some of these antimicrobial peptides are also widely used in livestock production, both for infection control and growth promotion. This raised concerns that agricultural use could lead to cross-resistant bacteria that could overcome the human innate immune response.

In the new study, led by the University of Oxford, researchers have shown that the evolution of such cross-resistant bacteria is not only possible, but highly probable.
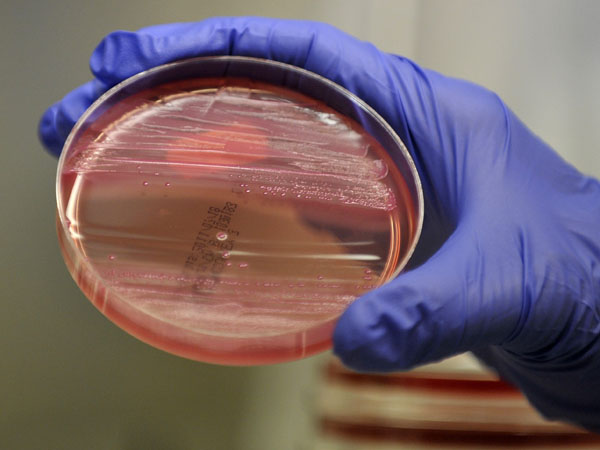
To test the idea, the researchers used colistin, which is an antimicrobial peptide produced by bacteria (Bacillus polymyxa) that is chemically and functionally similar to those produced in animals.
Colistin has become increasingly important as a “last line of defense” in the treatment of infections caused by multi-resistant bacteria. However, the extensive use of colistin in livestock production since the 1980s has fueled the spread of bacteria. Escherichia coli carriers of colistin resistance (MCR) genes.
E. coli bacteria carrying an MCR gene (MCR-1) were exposed to antimicrobial peptides known to play an important role in innate immunity in chickens, pigs, and humans.
The sensitivity of the bacteria to human serum, which contains a complex cocktail of antimicrobial compounds, and their ability to infect wax moth larvae (melonella gallery).
On average, the MCR-1 gene increased the host organism’s resistance to antimicrobial peptides by 62%, compared to bacteria lacking the gene. This increase in resistance provided a strong selective advantage to the MCR-1 gene in the presence of antimicrobial peptides.
Similarly, bacteria Escherichia coli MCR-1 carriers were at least twice as resistant to killing by human serum. E. coli strains carrying the MCR-1 gene were more virulent in wax moth larvae than control strains lacking the gene.
Larvae injected with the bacteria E.coli MCR-1 showed approximately 50% lower survival than larvae injected with E.coli of control. The results demonstrate that the use of antimicrobial peptides in agriculture can generate extensive cross-resistance to the human innate immune response.
According to the researchers, cross-resistance to human antimicrobial peptides is likely to be widespread, as they often have similar cellular targets and physicochemical properties.

It is already known that pigs and chickens act in agriculture as important reservoirs of E.coli colistin resistant.
According to Professor Craig MacLean, Principal Investigator, the study “clearly shows that the anthropogenic use of antimicrobial peptides such as colistin can drive the accidental evolution of resistance to the innate immune system of humans and animals.”
That risk has important implications for the design and use of peptide therapeutics and suggests that resistant genes may be difficult to eradicate, even if the use of antibiotics in agriculture is withdrawn, the scientist said.
“Antimicrobial peptides have been championed as a promising alternative to antibiotics to treat bacterial infections,” he stated. But he considered that “using them in this way will lead to the evolution of resistance to the peptides in pathogenic bacteria,” according to the expert.

“Our results -he remarked- provide strong evidence that we will need to adequately assess the impact of resistance to new therapeutic antimicrobial peptides on bacterial virulence before they are used to treat patients. Otherwise, we will run the risk of accidentally arming pathogenic bacteria against our own immune system,” she warned.
consulted by infobae, Alejandro Vila, a researcher at the Institute of Molecular and Cellular Biology of Rosario, which depends on Conicet in Argentina, said that the results of the Oxford work are interesting. “They show that when the bacterium has a resistance gene, it has synergy that enhances infectivity in the organism,” he commented.
Cóilín Nunan, scientific adviser to the Alliance to Save Our Antibiotics (who was not involved in the study), stated: “This new study shows that colistin resistance is probably even more dangerous than previously thought. It is astonishing that so many governments, such as the UK, refuse to ban the use of colistin in agriculture.” In other countries, such as Argentina, it is prohibited (it was decided in 2019).

Meanwhile, Dr. Jessica Blair, from the University of Birmingham and editor-in-chief of NPJ Antimicrobials and Resistance (who was not involved in the study), opined:
“Antimicrobial peptides, including colistin, have been heralded as a potential part of the solution to the rise in multidrug-resistant infections. However, this study suggests that resistance to these antimicrobials may have unintended consequences on the ability of pathogens to cause infection and survive in the host. This is especially worrisome because it suggests that the bacterium Escherichia coli carrier of the MCR-1 gene may have a clear selective advantage even if colistin use is carefully controlled.”
Keep reading:

