Transverse myelitis is inflammation on both sides of a section of the spinal cord. This neurological disorder often damages the insulating material that covers nerve cell fibers (myelin).
Transverse myelitis interrupts the messages that the nerves in the spinal cord send throughout the body. This can cause pain, muscle weakness, paralysis, sensory problems, or bladder and bowel dysfunction.
There are many different causes of transverse myelitis, including infections and disorders of the immune system that attack the body’s tissues. It can also be caused by other myelin disorders, such as multiple sclerosis. Other conditions, such as a spinal cord stroke, are often confused with transverse myelitis, and these conditions require other treatment approaches.
Treatment for transverse myelitis includes medication and rehabilitation therapy. Most people with transverse myelitis make at least a partial recovery. People with severe seizures are sometimes left with significant disabilities.
The signs and symptoms of transverse myelitis usually occur over a few hours to a few days and can sometimes gradually progress over several weeks.
Transverse myelitis usually affects both sides of the body below the affected area of the spinal cord, but sometimes there are symptoms on only one side of the body.
Typical signs and symptoms include:
Pain. The pain from transverse myelitis can start suddenly in the lower back. The sharp pain may go down the legs or arms, or around the chest or abdomen. Pain symptoms vary depending on the part of the spinal cord that is affected.
abnormal sensations Some people with transverse myelitis report having numbness, tingling, cold, or burning sensations. Some are especially sensitive to the light touch of clothing or to extreme heat or cold. You may feel as if something is squeezing the skin on your chest, abdomen, or legs.
Weakness in the arms or legs. Some people notice heavy legs, or that they are stumbling or dragging one foot. Others may have severe weakness or even total paralysis.
Bladder and bowel problems. This can include the need to urinate more often, urinary incontinence, difficulty urinating, and constipation.
Call your doctor or seek emergency medical attention if you are experiencing signs and symptoms of transverse myelitis. Various neurological disorders can cause sensory problems, weakness, and bladder or bowel dysfunction, including spinal cord compression, which is a surgical emergency.
Another less common cause is a spinal cord stroke due to poor blood circulation. This can be caused by blockage of a blood vessel that supplies blood to the spinal cord, which can occur with surgery to the aorta or increased blood clotting. It is important to get a timely diagnosis and appropriate treatment.
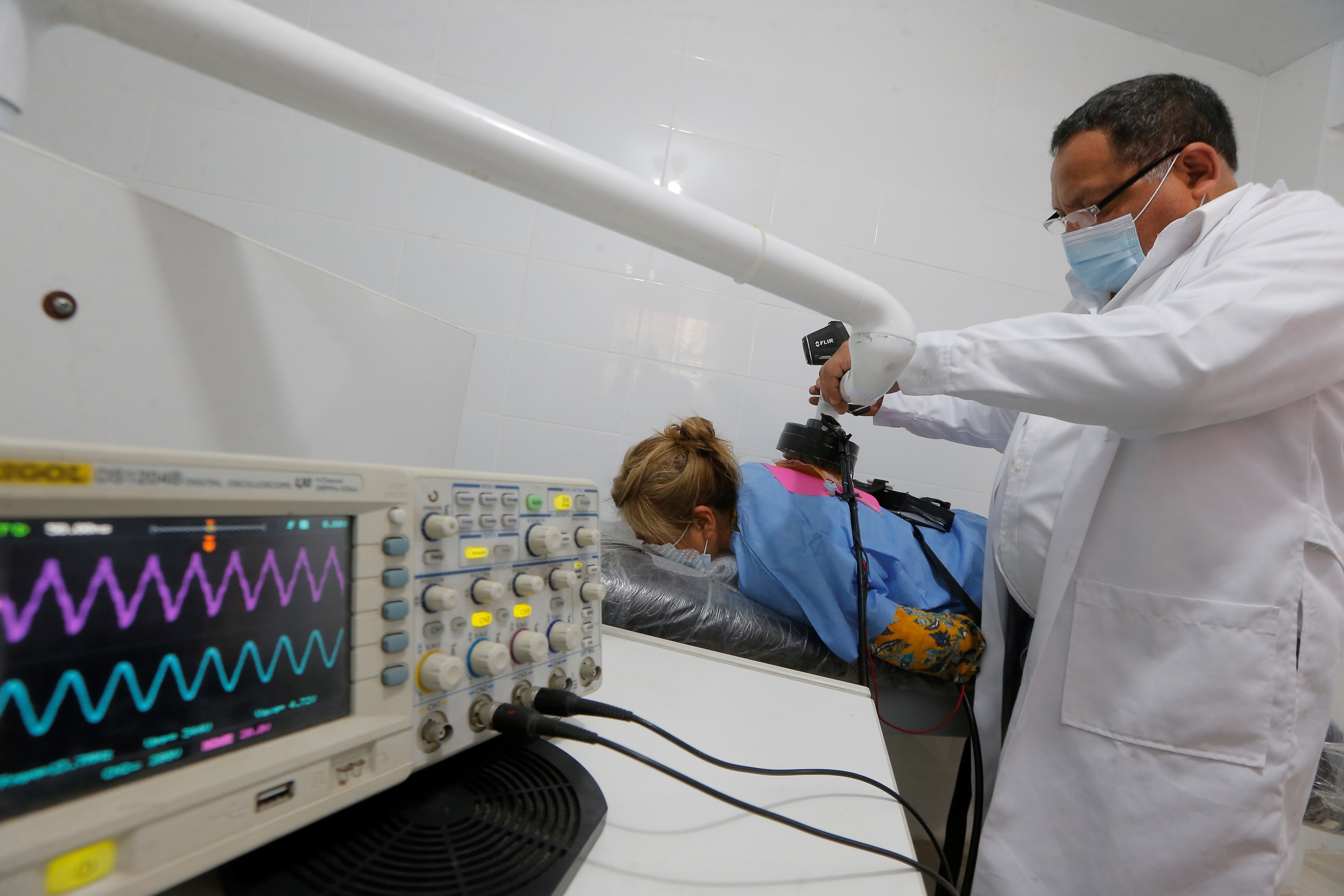
A doctor will diagnose transverse myelitis based on your answers to questions about your signs and symptoms, your medical history, a clinical assessment of nerve function, and test results.
These tests, which can indicate inflammation of the spinal cord and rule out other disorders, include the following:
On the MRI a magnetic field and radio waves are used to create 3D images of soft tissue. A magnetic resonance it can indicate inflammation of the spinal cord and other possible causes of symptoms, including abnormalities affecting the spinal cord or blood vessels.
In the lumbar puncture A needle is used to remove a small amount of cerebrospinal fluid, the protective fluid that surrounds the spinal cord and brain. In some people with transverse myelitis, the cerebrospinal fluid You may have abnormally high numbers of white blood cells or immune system proteins that indicate inflammation. Cerebrospinal fluid may also be tested for viral infections or certain types of cancer.
blood tests They may include testing for antibodies associated with neuromyelitis optica, a condition in which inflammation occurs in both the spinal cord and the eye nerve. People who test positive for antibodies are at increased risk of having multiple attacks of transverse myelitis and require treatment to prevent future attacks. Other blood tests can detect infections likely to contribute to transverse myelitis or rule out other causes of symptoms.
Many therapies focus on the acute signs and symptoms of transverse myelitis:
intravenous steroids. You will probably receive steroids through a vein in your arm over the course of several days. Steroids help reduce inflammation in the spine.
Plasma exchange therapy. People who do not respond to intravenous steroids may need plasma exchange therapy. It consists of extracting the straw-colored liquid in which the blood cells (plasma) are suspended and replacing the plasma with special liquids. It is not known for sure how this therapy helps people with transverse myelitis, but it is possible that plasma exchange removes inflammatory antibodies.
Antiviral drugs. Some people who have a viral infection of the spinal cord may be given medicines to treat the virus.
Analgesics. Chronic pain is a common complication of transverse myelitis. Medications that can decrease muscle pain include common pain relievers such as acetaminophen (Tylenol, others), ibuprofen (Advil, Motrin IB, others), and naproxen sodium (Aleve). Nerve pain can be treated with antidepressant medications, such as sertraline (Zoloft), and anticonvulsants, such as gabapentin (Neurontin, Gralise) or pregabalin (Lyrica).
Medications to treat other complications. Your doctor may prescribe other medications as needed to treat problems such as muscle spasticity, urinary or bowel dysfunction, depression, or other complications associated with transverse myelitis.
Medications to prevent recurrent attacks of transverse myelitis. People who have antibodies associated with neuromyelitis optica need ongoing medications, such as corticosteroids or immunosuppressants, to reduce their chances of having more attacks of transverse myelitis or optic neuritis.
Other therapies focus on recovery and long-term care:
Physiotherapy. This helps improve strength and coordination. The physical therapist can teach you how to use any assistive devices you need, such as a wheelchair, canes, or braces.
occupational therapy. This helps people with transverse myelitis learn new ways to do daily activities, such as bathing, preparing food, and doing chores.
Psychotherapy. A psychotherapist can use talk therapy to treat anxiety, depression, sexual dysfunction, and other emotional and behavioral problems that arise from coping with transverse myelitis.
Although most people with transverse myelitis make at least a partial recovery, it can take a year or more. Most recovery occurs within the first three months after the episode and is highly dependent on the cause of the transverse myelitis.
About a third of people with transverse myelitis fall into one of three categories after an attack:
No or slight disability. These people experience only minimal persistent symptoms.
Moderate disability. These people are mobile, but may have difficulty walking, numbness or tingling, and bladder and bowel problems.
severe disability. Some people may permanently need a wheelchair and require ongoing assistance with care and daily activities.
It is difficult to predict the course of transverse myelitis. Prognosis and responsiveness to treatment are strongly determined by the cause of the syndrome and, to some extent, by how early treatment is delivered. Generally, people who experience a rapid onset of severe signs and symptoms and those who test positive for a particular antibody have a worse prognosis than those who have a relatively slower onset, milder symptoms, and a negative antibody test.
